What is salt and how does it affect our blood pressure?
Last Updated : 10 February 2023Salt has been used to flavour and preserve foods for thousands of years. We all need some salt for good health, but eating too much can increase our blood pressure, increasing our risk of heart disease. Here we discuss how too much salt can increase blood pressure, the relationship between salt and high blood pressure across Europe and what we can do to reduce our salt intake.
What is salt?
Salt is the common name for sodium chloride (or NaCl). It consists of 40% sodium and 60% chloride. In other words, 2.5 g of salt contains 1 g of sodium and 1.5 g of chloride.
Why do we need salt?
Both sodium and chloride are essential for many body functions. They help regulate blood pressure, control fluid balance, maintain the right conditions for muscle and nerve function and allow for the absorption and transport of nutrients across cell membranes. Chloride is also used to produce stomach acid (hydrochloric acid, HCl), which helps us digest foods.
How much salt do we need per day?
The exact minimum daily requirement for salt is unknown, but it is thought to be around 1.25 g – 2.5 g (equivalent to 0.5 – 1 g sodium) per day.1 As salt is found in a large variety of foods the risk of deficiency is low.1,2 The European Food Safety Authority (EFSA) has stated that a salt intake of 5 g per day (equivalent to 2 g of sodium) is sufficient to meet both our sodium and chloride requirements as well as reduce our risk of high blood pressure and heart disease.1,2 This is equivalent to around 1 teaspoon of salt per day from all sources.
Both sodium and chloride are released from our body through our urine and when we sweat. This means bouts of heavy sweating, such as during exercise, can increase our salt requirements slightly. However, as most people consume well above the required levels, it is usually not necessary to increase salt intake during these conditions.1
How much salt do people eat in Europe?
The average intake of salt varies across Europe, ranging from between 8 to 12 g per day.1 Across most European countries, both men and women, on average, consume well above recommended levels (figure 1). Men will often consume more salt than women as they tend to consume more food overall.
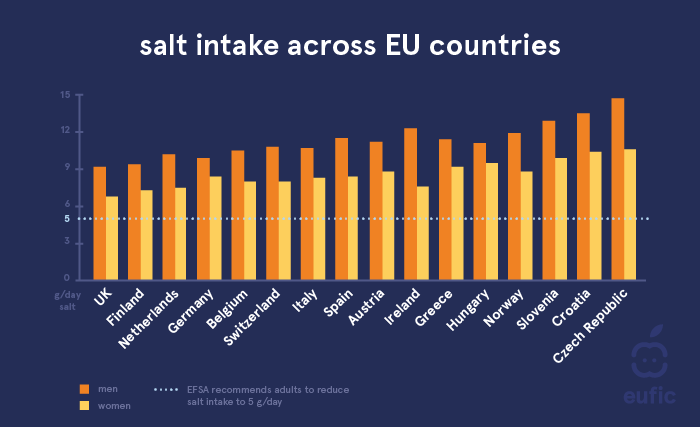
Figure 1. Estimated salt intake of men and women across European countries.1 Estimated salt intake was calculated from 24-hour urinary sodium using the equation 17.1 mmol of sodium = 1g of salt and assumes all sodium was derived from salt. For Ireland and German,y salt intake was calculated using spot urinary sodium, which means the result may be less reliable.
What is blood pressure?
Blood pressure is the measure of the force the heart uses to pump blood around the body. There are two different measures, systolic blood pressure (the highest pressure on blood vessels when the heart pushes blood out), and diastolic blood pressure (the lowest pressure on blood vessels when the heart relaxes between beats). Both are measured in millimetres of mercury (mmHg) and are often presented as a ratio of systolic/diastolic (e.g., 120/80 mmHg).
In general, healthy blood pressure is thought to be between 90/60 mmHg and 120/80 mmHg. High blood pressure (also known as hypertension) is often defined as a measurement of 140/90mmHg or higher and is a risk factor for many diseases, especially heart disease and stroke.3
Table 1. Blood pressure categories.3
|
Blood Pressure Category |
Systolic (mmHg) |
Diastolic (mmHg) |
|
Low blood pressure |
<90 |
<60 |
|
Optimal |
90-120 |
60-80 |
|
Normal |
120-129 |
80-84 |
|
High normal (elevated/prehypertension) |
129-139 |
85-89 |
|
High blood pressure (hypertension) |
≥140 |
≥90 |
How common is high blood pressure (hypertension) in Europe?
In 2015, an estimated 1.13 billion people were living with high blood pressure globally, of which 150 million were living in Europe (approximately 23.2% of the population).4 Although the prevalence (% of the population) of high blood pressure in many European countries has decreased slightly in recent years, current levels are still of great concern. Reducing salt intake remains an important public health strategy to decrease levels further.
As with salt intake, the prevalence of high blood pressure tends to be higher for men than for women (figure 2). The exact reason for this difference is not fully understood, but higher intakes of salt may be partly to blame.
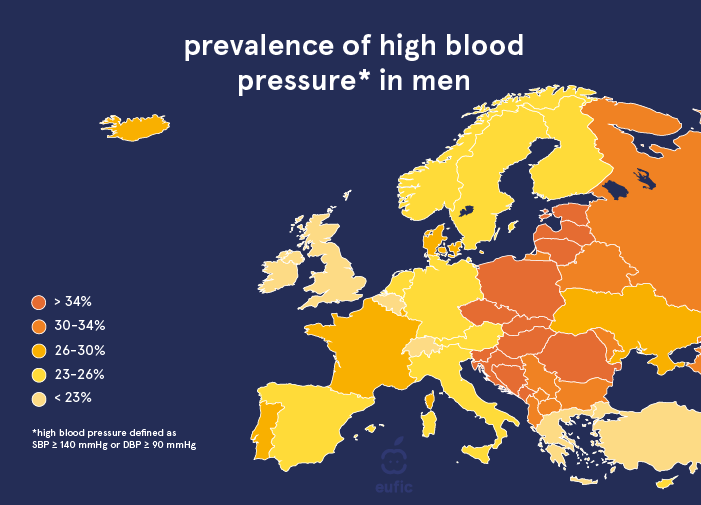
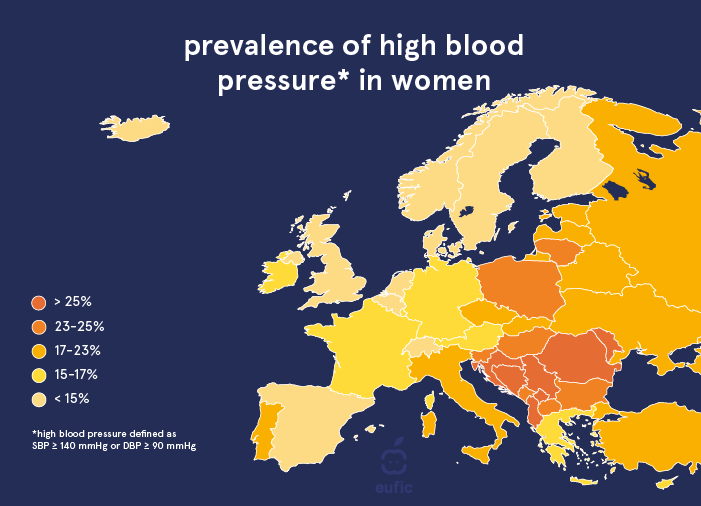
Figure 2. Prevalence (% of the population) of high blood pressure (defined as systolic blood pressure (SBP) ≥140 mmHg OR diastolic blood pressure (DBP) >90 mmHg) in men and women across European countries.4
How does salt increase our blood pressure?
Normally our kidneys do a good job at regulating the sodium and water levels of our blood. However, for many of us, eating too much salt can disturb this balance, causing sodium levels in the blood to increase. This leads our body to hold onto more water and increases both the fluid surrounding our cells and the volume of blood in our bloodstream. As blood volume increases, the pressure on our blood vessels begins to increase and our heart needs to work harder to move blood around our body. Over time this extra strain can lead to the stiffening of blood vessels and increases the risk of high blood pressure, heart disease and stroke.
Does reducing salt improve our blood pressure?
There is consistent evidence that moderate reductions (i.e., a decrease of 3 to 5 g or ½ to 1 teaspoon a day) in salt intake can lead to a reduction in blood pressure.5,6 However, these effects may not be the same for everyone and will depend on an individual’s starting blood pressure (greater benefits are seen in those with higher blood pressure), their current level of salt intake, genetics, disease status and medication use.
Salt is not the only lifestyle factor that can influence our blood pressure. Other factors such as eating enough potassium, maintaining a healthy body weight, not smoking, and being physically active are also important. You can find 7 lifestyle tips to help reduce blood pressure here.

Figure 3. Tips to improve blood pressure.
Should we all eat less salt?
Salt intake in Europe and across the globe is well above recommended levels and reducing salt is encouraged by most dietary guidelines. Individually, most of us could benefit from reducing our salt intake and at a population level, this can also have a significant benefit to public health.7 To reach the 5 g of salt per day recommendation set by EFSA, both individuals and the food industry will need to commit to improving dietary choices and reducing the salt content of products, respectively.
Many EU countries have made progress in industry-led salt reduction campaigns, but more work is needed if we want to reach the target set by EFSA.8 There also remain some key challenges to improving public knowledge and awareness on the importance of salt reduction. These include increasing awareness on the recommended intake, which food sources contribute most and educating people on how to read nutrition information on food labels.9
5 tips to reduce salt intake
Most of the salt we consume comes from ready-to-eat convenience foods, as well as foods prepared outside of the home. Here are some tips to help you reduce your salt intake:
- Avoid adding salt to foods or use reduced-sodium table salts.
- Even foods that don’t taste salty such as breakfast cereals or bread can be high in salt. Always check the nutritional information and choose low salt varieties when possible (figure 4).
- Choose unsalted nuts, seeds and other snack foods instead of salted varieties.
- Use herbs and spices instead of salt to flavour foods.
- Be conscious of foods eaten outside of the home and ask for less salt where possible.
High salt foods:
- Processed meats such as bacon, salami, sausages and ham
- Cheeses
- Gravy granules, stock cubes, yeast extracts
- Olives, pickles and other pickled foods
- Salted and dry-roasted nuts and crisps
- Salted and smoked meat and fish
- Sauces: soy sauce, ketchup, mayonnaise, BBQ sauce

Figure 4. How much salt is too much? Salt is just one nutrient we need to look out for on nutrition labels, for more information, see our infographic on understanding nutrition information.
References
- European Food Safety Authority., 2019. Dietary reference values for sodium. EFSA Journal, 17(9):5778.
- European Food Safety Authority., 2019. Dietary reference values for chloride. EFSA Journal, 17(9):5779.
- Williams, B., et al. 2018. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European heart journal, 39(33), pp.3021-3104.
- NCD Risk Factor Collaboration, 2017. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19· 1 million participants. Lancet (London, England), 389(10064), p.37.
- He, F.J., Li, J. and MacGregor, G.A., 2013. Effect of longer‐term modest salt reduction on blood pressure. Cochrane database of systematic reviews, (4).
- Huang, L., et al., 2020. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ, 368.
- Hendriksen, M.A., et al. 2017. Identification of differences in health impact modelling of salt reduction. PloS one, 12(11), p.e0186760.
- Trieu, K., et al., 2015. Salt reduction initiatives around the world–a systematic review of progress towards the global target. PloS one, 10(7), p.e0130247.
- Bhana, N., Utter, J. and Eyles, H., 2018. Knowledge, Attitudes and Behaviours Related to Dietary Salt Intake in High-Income Countries: a Systematic Review. Current nutrition reports, 7(4), pp.183-197.
