What is the role of gut bacteria in human health?
Last Updated : 15 November 2024
Your body is home to trillions of microorganisms, including bacteria, yeasts, and viruses, which live in various areas such as your skin, nose, mouth, and gut. Many of these microorganisms reside in your gut, and among these, the bacteria there play a particularly important role in regulating your health through hormone regulation, metabolism regulation, immune response, and digestion. But that’s not all – gut bacteria are linked to a range of health conditions, from metabolic diseases like obesity and type 2 diabetes, to mental health disorders. In this article, we explore what gut bacteria are and how they affect our overall health.
What are gut bacteria?
The human gastrointestinal tract is home to a vast community of over 100 trillion microorganisms, mainly bacteria. One of the many jobs of these bacteria is to help us digest and use the nutrients from our food. They also serve other important functions that regulate our overall health, such as supporting our immune system1 .
Each person has a unique community of microorganisms living in their gut – this is called the gut microbiota. The gut microbiota is first influenced by genetics and birth, but changes throughout a person’s life due to factors like diet, age, geographical location, and the use of certain medications, like antibiotics 2,3. The gut microbiota, together with its genetic material and associated metabolites living in the intestinal tract, is called the gut microbiome.
While there isn’t a consensus definition of a “healthy gut microbiome” – partly because everyone’s microbiome is unique (even identical twins!) and because your microbiome changes throughout your lifetime – there are certain indicators that can help us understand features that contribute to positive or negative health outcomes. Importantly, we know that having a lot of diversity in our gut bacteria makes our microbiome more capable and resilient2. In adults, a microbiome with many different types of bacteria works more effectively than one with only a few types, because if one bacteria can't do its job, another can take over.
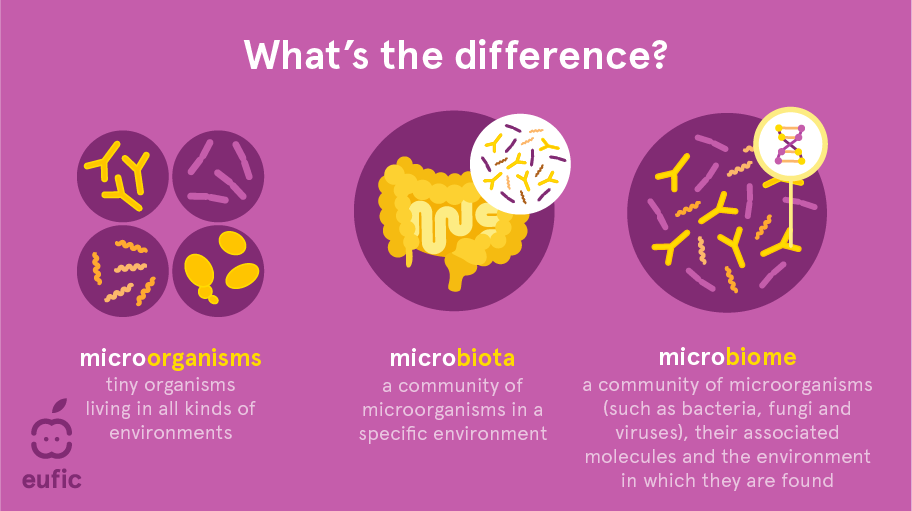
Fig 1 – Illustration of the difference between microorganisms, microbiota, microbiome
How do gut bacteria impact our health?
Our gut bacteria support many essential body functions, including vitamin production and nutrient absorption, immune system response, hormone regulation, metabolism regulation, and protection against harmful pathogens 4.
When the balance of microorganisms in the gut is disrupted, it can negatively impact these functions, and a condition known as dysbiosis may occur. Gut dysbiosis has been linked to health issues including allergies, autoimmune diseases, certain cancers, asthma, metabolic diseases like type 2 diabetes and obesity, and mental health disorders like anxiety and depression1. However, it is still unclear whether the changes in gut bacteria cause these diseases or are a result from them4.
Researchers have also found that people with certain diseases often have different kinds of bacteria living in their gut compared to those who do not have the disease. For instance, individuals with inflammatory bowel disease (IBD) or type 2 diabetes tend to have gut microbiota that is noticeably different from those without these conditions.
How do gut bacteria affect our immune system?
A large part of our immune system, about 70-80% of the body's immune cells, is found in the gut. Here, the immune cells continuously interact with gut bacteria. This close relationship is crucial for shaping the immune system because it helps to create, develop, and regulate various immune cells, while also protecting against harmful pathogens. In return, immune cells help stabilise the balance of gut microorganisms. This partnership is vital for maintaining stability in the immune system and keeping the body healthy. However, if the structure and function of gut microbiota are disrupted, it can lead to an overgrowth of harmful bacteria, increasing the risk of infections and other health problems3.
Can gut bacteria affect mental health?
There is a significant connection between the gut and the brain, commonly referred to as the ‘gut-brain axis’. This two-way communication system means that the gut can influence cognitive performance, mood, and behaviour. For example, gut-related issues like irritable bowel syndrome (IBS) can affect what’s happening in the brain, and vice-versa, stress is a major trigger for IBS symptoms and the disease is closely related to anxiety disorders, early-life trauma or depression 5,6. Hence, our mind and mental health can have a significant impact on our gut – expanding our understanding of mental health beyond just the brain itself 7,8.
Several studies suggest that the diversity and composition of gut microbiota play a role in conditions like depression, anxiety, and other psychological disorders. Research is also exploring the role of gut microbiota in the progression of neurological disorders such as Alzheimer’s, cerebrovascular stroke, Parkinson’s disease, and schizophrenia4,9.
New research is investigating how improving gut microbiome functions could support better mental health. For example, existing clinical trials have demonstrated that probiotics, beneficial bacteria that influence the gut-brain link, might help reduce anxiety, improve mood, and even enhance cognitive function in conditions like bipolar disorder . This has led to the term 'psychobiotic' to describe how probiotics (and prebiotics) might relieve mental health symptoms8,9,10.
Dietary patterns, which strongly impact gut microbiota, are also being studied for their impact on mental health . For instance, high-fat diets rich in animal products have been shown to disrupt the balance of gut microorganisms, while on the other hand, the Mediterranean diet (rich in fibre and prebiotics from whole grains, nuts, and vegetables) has been linked to reducing the occurrence of psychiatric conditions and the risk of depression4,11.
How do gut bacteria influence weight loss?
Many studies have identified significant links between gut bacteria, weight gain, and obesity. Our gut bacteria help regulate body weight by influencing energy levels, appetite, how we absorb nutrients, and the function of adipose tissue which impacts how our bodies store fat5,12, 13. For example, in people with obesity, gut bacteria are better at extracting energy from food compared to those with a normal weight. Notably, people with obesity often have less diverse gut bacteria and different types of gut bacteria compared to those without obesity – and the types of bacteria found in the gut can vary depending on how severe the obesity is 14,15. An imbalance in gut bacteria can both contribute to the development of obesity by affecting metabolism and fat storage, and it can also result from obesity, where gut bacteria becomes disbalanced from the impact of weight gain1. The development of the microbiota in early childhood can also influence a child’s growth and risk of obesity later in life.
Much of the evidence linking gut bacteria and obesity comes from animal studies. Many studies have been carried out with humans, but are limited due to underrepresented populations and outcomes with opposing results15. Existing studies have shown associations between changes in gut bacteria – like those caused by antibiotics – and the development of weight gain1,16. As findings from animal studies cannot be directly applied to humans, more research is necessary to understand how, and to what extent, the gut microbiome may impact human metabolism .
Modifying the gut microbiota composition through diet, probiotics or prebiotics has shown promise as a weight management strategy. Personalised approaches and combined interventions may be necessary to see improvements for individuals . Importantly, it’s crucial that any microbiome-related treatments should be conducted under professional medical guidance to ensure they are safe and effective.
-> Research highlight: The EU-funded BETTER4U project is working to develop personalised interventions to address obesity and weight gain. The project aims to understand how factors like genetics, epigenetics, lifestyle, environment, and the gut microbiome influence weight gain and to identify potential microbial strains that could aid in weight loss.
What factors influence the composition of gut bacteria?
Birth mode and early life
The gut microbiome begins to form early in life. How a baby is born – whether through vaginal delivery or caesarean section – can influence the types of bacteria that settle in their gut. Babies born through vaginal delivery mainly get their gut bacteria from the mother’s vaginal bacteria. Babies born via caesarean section pick up different bacteria from the surrounding environment, for example from the mother’s skin, the medic’s skin, and the surrounding environment. This tends to impact the composition of the gut microbiota in infants for up to 6 months after birth16.
Feeding is also an important factor in the development of an infant’s microbiota, whether it is breastfeeding or formula feeding. Human milk is rich in essential nutrients such as fats, proteins, carbohydrates, and immunoglobulins, all which support microbiota diversity. Improvements in infant milk formula, such as the addition of specific oligosaccharides, aim to promote a microbiota rich in beneficial bacteria strains that are linked to positive health outcomes. As an infant grows, their microbiota evolve, and by the time they reach three years of age the gut microbiota becomes quite similar to an adult's 19,20.
Effects of antibiotics
Antibiotics help us combat (life-threatening) bacterial infections, however, while doing so, they can also harm beneficial microorganisms in our gut. Antibiotics reduce microbial diversity and alter functional attributes of the gut microbiome, which can lead to dysbiosis21. The extent of these changes depends on several factors, such as the specific antibiotic used, dosage, and period of use17. While the impact of antibiotics is usually short-term, disturbances of the gut microbiota for extended periods of times have also been documented, with some cases associated with increased risk of asthma, food allergies, or weight gain 21.
Antibiotic usage can lead to mild or more severe cases of diarrhoea, caused by the pathogen Clostridioides difficile. Taking probiotics during antibiotic treatment can reduce the risk of developing antibiotic-associated diarrhoea .
It is important to be aware of the dangers of use, misuse and abuse of antibiotics23. Only take antibiotics when prescribed by your doctor (and not self-medicate), follow your GP's advice and finish the whole prescription.
Diet and lifestyle
Diet and lifestyle have a major impact on shaping the composition and function of our gut bacteria in the long-term19,23 . Gut bacteria highly depend on the foods we eat, which can either help or harm their functioning. For example, gut bacteria ferment non-digestible substrates such as dietary fibres (for example, prebiotics), a process that produces short-chain fatty acids, which are important for regulating metabolism and inflammation, and reducing the risk of disease13,24. In general, diets rich in high-fibre, plant-based foods, and whole grains help support a diverse microbiome. In contrast, diets characterised by low-fibre foods can reduce microbial diversity12.
Consuming probiotics or prebiotics, either in the form of supplements or via certain foods, can improve intestinal health as they promote the presence of beneficial gut bacteria26. Probiotic treatments have the potential to restore gut dysbiosis by limiting the growth of harmful bacteria and strengthening the functions of the gut barrier1,21. It is for this reason that probiotics have been studied in clinical trials for their therapeutic potential in treating a wide range of health conditions, from type 2 diabetes and obesity to mental health disorders.
In terms of lifestyle factors, regular physical exercise, interacting with pets, spending time in nature and getting adequate sleep can all foster a diverse and healthy microbial community in the gut. On the other hand, exposure to environmental pollutants, smoking and drinking too much alcohol can reduce microbial diversity and disrupt the balance between beneficial and harmful bacteria. This can lead to increased inflammation and a higher risk of disease. Managing stress is also important, as chronic stress can negatively impact digestion, reduce the presence of beneficial bacteria, and cause problems in the gut barrier, leading to inflammation 25,26.

Fig. 2 – What factors influence the gut microbiota?
What foods help promote healthy gut bacteria?
Overall, a balanced diet rich in a diversity of fruits and vegetables, fermented products with live microorganisms, and healthy fats (i.e., unsaturated fats) is key to fostering a diverse gut microbiome. Some foods that can support a healthy gut include:
- High-fibre foods: fruits, vegetables, and whole grains like berries, leafy greens, and quinoa are great sources of fibre. These increase the presence of diverse and beneficial bacteria, while also providing essential nutrients.
- Fermented foods: some fermented foods like yoghurt, kefir, kimchi, and sauerkraut contain live microorganisms, and are often rich in probiotic bacteria. Eating these can introduce healthy bacteria directly into your gut.
- Foods high in prebiotics: prebiotics act as food for your beneficial gut bacteria, they can be found in a range of food sources, like chicory, chia seeds, flaxseeds, onion, garlic, almonds, artichoke, oats, and many plants 27.
- Polyphenol-rich foods: fruits like raspberries, blueberries, oranges, grapes, pomegranate, pineapple and grapefruit; vegetables like eggplants, chilis; nuts like hazelnut and chestnut; tea (such as green, black and oolong) and coffee are found to be rich in polyphenols, which can promote the growth of beneficial microorganisms 28,29,30.
- Foods rich in omega-3 and omega-6 fatty acids: walnuts, flaxseeds, and oily fish, like salmon, mackerel and sardines, have anti-inflammatory properties that help maintain a balanced gut environment.
Foods that are high in saturated fat, such as fried foods, and foods high in added and free sugars, like soft drinks and sweets, can negatively impact gut bacteria . Try swapping potato chips with raw veggies and hummus or replacing a sugary dessert with a bowl of fresh fruit salad.
-> Research highlight: The EU funded DOMINO project is researching the impact of fermented foods on the gut microbiome, and the links to health benefits. This project will contribute to a better understanding of how dietary recommendations based on fermented foods can support recovery for individuals with metabolic syndrome.
Conclusion
The bacteria living in the human gut are crucial for human health. Exactly how, to what extent, and what areas of human health are influenced by our microbial “inhabitants” is an exploding area of research. While gaps in the knowledge remain, there are well-established links showing that gut bacteria influence the way we function: from digestion and immune function to mental health and weight management. The balance and diversity of gut bacteria, which indicates how well a microbe community functions, is shaped by a complex interplay of factors, including diet, lifestyle, genetics, epigenetics, and microbial exposure in early life. Maintaining a diverse gut microbiome through a balanced diet rich in fibre, fermented foods, and prebiotics, alongside positive lifestyle choices like regular exercise and stress management, can support not only digestive health but also contribute to reducing the risk of various chronic diseases.
This article was written in collaboration with EUFIC and researchers from the DOMINO and BETTER4U projects.
The DOMINO project has received funding from the European Union’s Horizon Europe research and innovation programme under grant agreement No 101060218.


The BETTER4U project has received funding from the European Union’s Horizon Europe research and innovation programme under grant agreement No 101080117.


References
- Fujisaka S, Watanabe Y & Tobe K (2023). The gut microbiome: a core regulator of metabolism. Journal of Endocrinology 256(3).
- Dogra SK, Doré J & Damak S (2020). Gut Microbiota Resilience: Definition, Link to Health and Strategies for Intervention. Frontiers in Microbiology 11:572921.
- Wiertsema SP, et al. (2021). The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients 13(3):886.
- Hou K, et al. (2022). Microbiota in health and diseases. Signal Transduction and Targeted Therapy 7(1):135.
- Sperber AD, et al. (2022). Greater Overlap of Rome IV Disorders of Gut-Brain Interactions Leads to Increased Disease Severity and Poorer Quality of Life. Clinical Gastroenterology and Hepatology 20(5).
- Parker CH, et al. (2019). Negative Events During Adulthood Are Associated With Symptom Severity and Altered Stress Response in Patients With Irritable Bowel Syndrome. Clinical Gastroenterology and Hepatology 17(11):2245-2252.
- Lucas G (2018). Gut thinking: the gut microbiome and mental health beyond the head. Microbial Ecology in Health and Disease 29(2).
- Bruce-Keller AJ, Salbaum JM & Berthoud HR (2018). Harnessing Gut Microbes for Mental Health: Getting From Here to There. Biological Psychiatry 83(3):214-223.
- Johnson D, et al. (2021). Exploring the Role and Potential of Probiotics in the Field of Mental Health: Major Depressive Disorder. Nutrients 13(5):1728.
- Ross FC, et al. (2024). The interplay between diet and the gut microbiome: implications for health and disease. Nature Reviews Microbiology.
- Losno EA, et al. (2021). Vegan Diet and the Gut Microbiota Composition in Healthy Adults. Nutrients 13(7):2402.
- Cani PD & Van Hul M (2024). Gut microbiota in overweight and obesity: crosstalk with adipose tissue. Nature Reviews Gastroenterology & Hepatology 21:164-183.
- Liu BN, et al. (2021). Gut microbiota in obesity. World Journal of Gastroenterology 27(25):3837-3850.
- Geng J, et al. (2022). The links between gut microbiota and obesity and obesity related diseases. Biomedicine & Pharmacotherapy 147:112678.
- Rinninella E, et al. (2019). What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms 7(1):14.
- Leong KSW, et al. (2018). Antibiotics, gut microbiome and obesity. Clinical Endocrinology (Oxford) 88(2):185-200.
- Pillai SS, et al. (2024). Exploring the Gut Microbiota: Key Insights Into Its Role in Obesity, Metabolic Syndrome, and Type 2 Diabetes. Journal of Clinical Endocrinology & Metabolism.
- Van Hul M & Cani PD (2023). The gut microbiota in obesity and weight management: microbes as friends or foe? Nature Reviews Endocrinology 19:258-271.
- san N & Yang H (2019). Factors affecting the composition of the gut microbiota, and its modulation. PeerJ 7.
- Ríos-Covian D, Langella P & Martín R (2021). From Short- to Long-Term Effects of C-Section Delivery on Microbiome Establishment and Host Health. Microorganisms 9(10):2122.
- Konstantinidis T, et al. (2020). Effects of Antibiotics upon the Gut Microbiome: A Review of the Literature. Biomedicines 8(11):502.
- Kopacz K & Phadtare S (2022). Probiotics for the Prevention of Antibiotic-Associated Diarrhea. Healthcare (Basel) 10(8):1450.
- Parizadeh M & Arrieta MC (2023). The global human gut microbiome: genes, lifestyles, and diet. Trends in Molecular Medicine 29(10):789-801.
- Fusco W, et al. (2023). Short-Chain Fatty-Acid-Producing Bacteria: Key Components of the Human Gut Microbiota. Nutrients 15(9):2211.
- Abdolghanizadeh S, et al. (2024). Microbiota insights into pet ownership and human health. Research in Veterinary Science 171:105220.
- Pedroza Matute S & Iyavoo S (2023). Exploring the gut microbiota: lifestyle choices, disease associations, and personal genomics. Frontiers in Nutrition 10:1225120.
- Kaur AP, et al. (2021). Plant Prebiotics and Their Role in the Amelioration of Diseases. Biomolecules 11(3):440.
- Wang X, Qi Y & Zheng H (2022). Dietary Polyphenol, Gut Microbiota, and Health Benefits. Antioxidants 11(6):1212.
- Plamada D & Vodnar DC (2022). Polyphenols—Gut Microbiota Interrelationship: A Transition to a New Generation of Prebiotics. Nutrients 14(1):137.
- Pérez-Jiménez J, et al. (2010). Identification of the 100 richest dietary sources of polyphenols: an application of the Phenol-Explorer database. European Journal of Clinical Nutrition 64(Suppl 3).
- Bolte LA, et al. (2021). Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut 70(7):1287-1298.