Obesity: definition, causes and prevention strategies
Last Updated : 17 October 2024Key takeaways:
- Obesity is a chronic, multifactorial disease involving excessive body fat that presents serious health risks.
- Obesity increases the risk of developing other non-communicable diseases, such as cardiovascular diseases, cancer, chronic respiratory diseases, diabetes mellitus, chronic kidney disease, nonalcholic fatty liver disease, musculoskeletal complications, and mental health problems.
- High-calorie diets and sedentary habits are major drivers of obesity, while genetics and underlying health conditions also play a role.
- Healthy habits throughout the life cycle, from weight management during pregnancy and healthy nutrition in childhood to maintaining a balanced diet, regular physical activity, and sufficient sleep, can help prevent obesity.
- Effective obesity management requires a coordinated, multisectoral effort involving governments, healthcare professionals, the food industry, educators, and consumers.
Obesity is a multifactorial, chronic, relapsing, non-communicable disease marked by an abnormal and/or excessive accumulation of body fat that presents a risk to health. It is well established that obesity acts as a gateway to a range of other non-communicable and communicable diseases. This article further explores the causes of obesity and explores prevention strategies.
What is obesity? Is obesity a disease?
Obesity is a chronic, multifactorial disease characterised by excessive or abnormal accumulation of adipose tissue (body fat) that poses significant health risks. The development of obesity is influenced by a complex interplay of genetic, physiological, environmental, and behavioural factors. Unlike conditions defined solely by visible symptoms or specific measurements, obesity involves intricate interactions between various factors, including genetics, physiology, and the environment.1
To help people determine what their healthy weight is, a simple measure of the relationship between weight and height called the Body Mass Index (BMI) is often used. BMI is a useful measurement that is commonly applied by doctors and other health professionals to determine the prevalence of underweight, overweight, and obesity. It is defined as the weight in kilograms divided by the square of the height in meters (kg/m2). Typically, a BMI of 18.5 to 24.9 is considered ‘healthy’, an individual with a BMI of 25–29.9 is considered overweight, and one with a BMI of 30 or more is considered as obese. For children and adolescents (aged >18 years old), pregnant women, as well as people of Asian, Chinese, Middle Eastern, Black African or African-Caribbean background different cut-offs are in place. 4
However, while BMI has been used as a simple tool for screening for underweight, overweight, and obesity in adults, it has large limitations. It does not fully account for the distribution of body fat or its implications for health. For instance, excess visceral fat, which accumulates around internal organs, is particularly associated with adverse health outcomes. Understanding obesity requires a nuanced view that goes beyond simple measure like BMI, considering the multifaceted nature of the condition and its broader implications for health and well-being. The European Association for the Study of Obesity (EASO) recommends that BMI, together with a waist-to-height ratio equal or larger than 0.5 and medical, functional or psychological impairment or complications, are used to diagnose obesity.1
The debate about whether obesity is a disease was historically complicated because there is not a single, agreed-upon definition of what a disease is. However, the classification of obesity as a disease is supported by leading health authorities such as the American Medical Association and the World Health Organization (WHO). This classifications reflects the serious health implications of obesity, including increased risk of morbidity and mortality, and underscores the need for comprehensive approaches to prevention and treatment.5
Obesity has many interlinked causes, including genetics, environment, and behaviour, making it essential to understand these factors for effective prevention and treatment. By recognising obesity as a disease, we can enhance our focus on effective prevention and treatment strategies, boost research efforts, and improve health promotion and insurance coverage. This approach fosters a more supportive and understanding societal attitude towards individuals living with obesity. It encourages the adoption of holistic and evidence-based treatment strategies that address the full spectrum of obesity’s impacts, rather than focusing solely on medical interventions. Emphasising a comprehensive and compassionate approach ensures that individuals receive the support they need to achieve their health goals and improve their well-being.
What is the difference between obesity and overweight?
The most common tool for differentiating between obesity and overweight is the BMI. For adults, the WHO defines overweight as having a BMI between 25 and 29.9 kg/m². Obesity is defined as having a BMI of 30 kg/m² or higher. 2
While both conditions increase the risk of health problems, the severity and variety of potential health issues are far greater in individuals with obesity. For instance, the accumulation of visceral fat is more common in individuals with obesity and strongly associated with poor health outcomes. 4
However, as mentioned above, understanding obesity requires a nuanced view that goes beyond simple measure like BMI, considering the multifaceted nature of the condition and its broader implications for health and well-being.
What causes obesity?
Obesity is a complex disease with many causes. Obesity and overweight result from an imbalance of energy intake (diet) and energy expenditure (physical activity sedentary behaviour), with extra calories being stored in the body as fat tissue. However, the causes of obesity are much more complex than just the combination of an unhealthy diet and physical inactivity.4 It is caused by the interaction between biological, genetic, social, psychological, policy-related and environmental factors.6
High-fat, energy-dense diets and sedentary lifestyles are the two characteristics most strongly associated with the increased prevalence of obesity worldwide.7 Our environment is one of the key components in promoting overweight and obesity by influencing these two characteristics. For example, our environments define whether there is availability of healthy, sustainable food at locally affordable prices, opportunities for people to engage in physical activity in daily life, and an adequate legal and regulatory environment. For instance, in urban areas with limited access to parks and recreational facilities, residents might find it difficult to engage in regular physical activity, contributing to a higher risk of obesity. Similarly, in areas where fast food is more accessible and affordable than fresh produce, individuals are more likely to consume unhealthy, energy-dense foods, leading to weight gain and obesity.
Genetics or underlying health conditions can also be a cause of obesity for some people. Genes affect how your body uses and stores fat. However, the role of genes is considered small compared to environmental factors like diet and physical activity. Certain medical conditions (e.g., hypothyroidism) and medications (e.g., some medicines for high blood pressure, diabetes or mental health conditions) can also make people more likely to gain weight.8
Which food causes obesity?
Not one single food is responsible for causing obesity. Obesity results from a complex interplay of various dietary patterns, genetic factors, and lifestyle choices. While foods high in calories, fats, and sugars can contribute to weight gain, it is the overall dietary habits and energy balance that play an important role in obesity. While the media may often point to carbohydrates or fat being responsible for the obesity epidemic, scientific evidence points to an overall caloric imbalance (e.g., regularly consuming more energy than we burn over long periods) contributing to weight gain.
Miracle or wonder diets that severely limit calories or restrict food groups should be avoided as they are often lacking important nutrients and/or cannot be sustained for prolonged periods. Besides, they do not encourage healthy or balanced eating habits and can result in yo-yo dieting (the gain and loss of weight in cycles resulting from dieting followed by over-eating). This so-called yo-yo effect may be dangerous to long-term physical and mental health.
When trying to lose weight, setting realistic goals is important. Even a modest weight loss of 10% of initial weight can bring significant health benefits.9 This approach is more sustainable and beneficial for long-term health compared to drastic dieting measures.
Is obesity genetic?
Genetics can play a role in the development of obesity. Research shows that the heritability of obesity is between 40% and 75%.10 Additionally, scientists have identified up to 500 genes related to obesity in humans. Specific genes linked to obesity can affect how the body stores fat, metabolises nutrients, signals feelings of fullness, and more.11 These genes can also influence hunger levels, food cravings, and the tendency to eat to cope with stress. Although there is strong evidence that genetics are linked to obesity, the role of genes is considered small compared to environmental factors like diet and physical activity. This means that what you eat and how much you move are bigger influences on obesity than genes alone.12
Some measures of obesity, such as BMI, waist-to-hip ratio, and skinfold thickness, show a high rate of heritability. However, the rapid increase in obesity levels in recent decades suggests that genes alone do not determine obesity. This increase has happened too quickly to be explained solely by genetics.
Is obesity a potential risk factor for certain health conditions?
Overweight and obesity are among the leading risk factors in the development of many non-communicable diseases (NCDs) and are also associated with early death. People living with overweight and obesity also face weight bias, stigma, discrimination, and challenges accessing empathetic, evidence-based healthcare.
Some medical conditions associated with obesity include 4:
- Cardiovascular diseases, including stroke, ischemic heart disease, heart failure, hypertensive heart disease, dyslipidaemia (abnormal high levels of lipids (fats) in the blood), and hypertension.
- Chronic respiratory diseases, including chronic obstructive pulmonary disease, obstructive sleep apnoea, and asthma.
- Cancer, including those of the breast, colorectum, gallbladder, stomach, kidney, liver, pancreas, uterus, ovary, oesophagus and thyroid, and multiple myeloma and meningioma.
- Chronic kidney disease.
- Mental health problems, such as depression.
- Musculoskeletal complications, including low back pain and osteoarthritis.
- Non-alcoholic fatty liver disease.
- Type 2 diabetes.
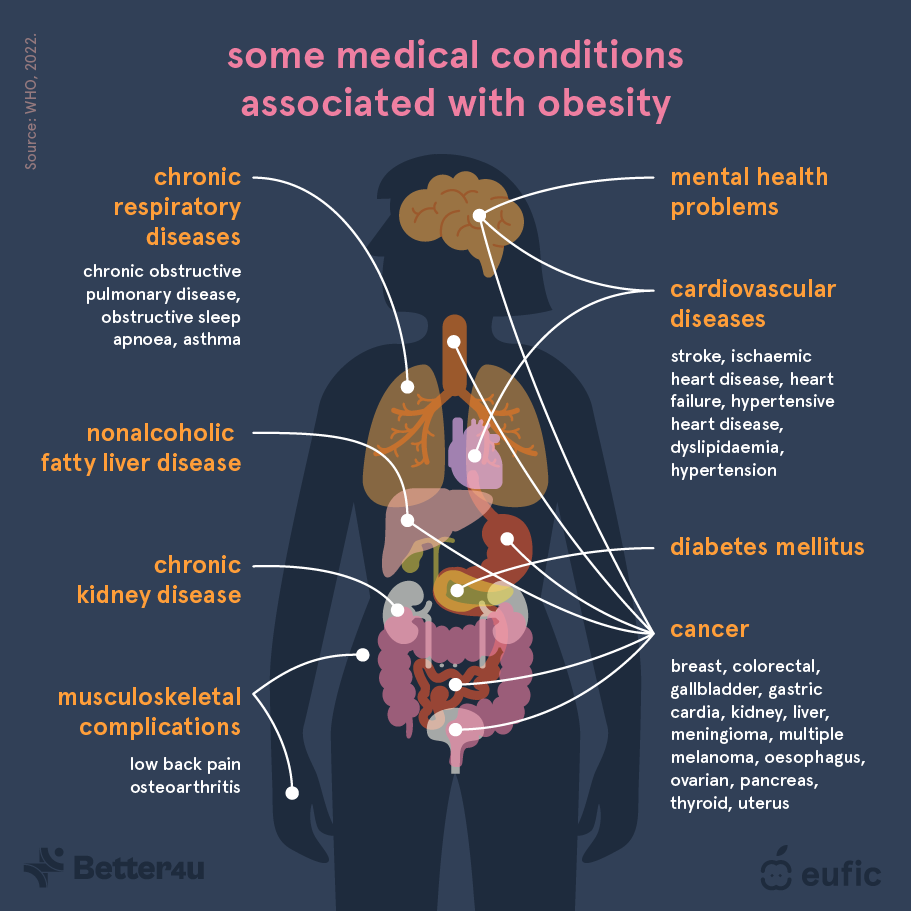
Fig. 1 – Medical conditions associated with obesity.1
Excess body weight and its distribution play an important role in determining health risks. Visceral fat, the type of fat which lies deep within the abdomen between our organs has been linked to various health conditions like type 2 diabetes, heart disease, and certain cancers.4 Visceral fat is more common in people with an ‘apple’ shape, i.e., people with more fat in the abdominal area. Subcutaneous fat, the type of fat which sits just underneath the skin, for example around the hips and thigh, but could also be in the abdominal area, is less dangerous but still contributes to health issues if present in large amounts.
People living with overweight and obesity often experience malnutrition, which may seem counterintuitive given that excess caloric intake is associated with obesity.13 However, this paradox is often due to eating high energy-dense, but low nutrient-dense foods, lacking essential nutrients like vitamins and minerals. Vitamin and mineral deficiency can compromise immune function, bone health, and cardiovascular health, leading to an increased risk of infections, osteoporosis, and heart disease.14
Type 2 diabetes
The risk of developing type 2 diabetes increases with a rising BMI, even if the BMI is below the cut-off point for obesity (BMI of 30).15 People living with obesity are more than seven and twelve times more likely, respectively, to develop type 2 diabetes compared to those of healthy weight.16
Obesity increases our risk of developing insulin resistance, where the body's cells become less responsive to insulin, the hormone that regulates our blood sugar levels. This forces the pancreas to produce more insulin, but over time it cannot keep up, resulting in high blood sugar levels. Additionally, obesity causes chronic inflammation because excess fat tissue releases substances that promote inflammation, further interfering with insulin's effectiveness.17
Hormonal imbalances also play a role. For instance, obesity often leads to higher levels of leptin, a hormone that reduces appetite, but also causes leptin resistance, making it less effective.18 Lower levels of adiponectin, a hormone that increases insulin sensitivity, are also common in people with obesity. These hormonal imbalances contribute to insulin resistance, a key factor in the development of type 2 diabetes. Leptin resistance can lead to increased food intake and further weight gain, while low adiponectin levels decrease the body's ability to manage blood glucose levels, both of which exacerbate the risk of type 2 diabetes.
Furthermore, excess fat can accumulate in organs like the liver and muscles, where it is not supposed to be, impairing their function and increasing insulin resistance.19 Lastly, the beta cells in the pancreas, which produce insulin, can become damaged from the constant high demand and exposure to high levels of fatty acids and inflammation, leading to decreased insulin production.20
Cardiovascular diseases
Obesity increases the risk of several cardiovascular risk factors, including high blood pressure, triglycerides (blood fats), and low-density lipoprotein (LDL) cholesterol.21 For example, women with obesity are about three times more likely to have a heart attack than those at a healthy weight.22 Excess body fat, particularly around the abdomen, leads to higher levels of triglycerides (blood fats) and low-density lipoprotein (LDL) cholesterol, commonly known as “bad cholesterol.” These factors contribute to the development of atherosclerosis, where arteries become narrowed and hardened due to the buildup of plaque, increasing the risk of heart attack and stroke.23
About 30-65% of high blood pressure cases in Western countries are attributed to obesity.24 For every 10 kg increase in weight, blood pressure can rise by 2-3 mm Hg. This means that even modest weight gain can push blood pressure into unhealthy ranges, increasing the risk of heart disease and stroke. Conversely, losing weight helps lower it. Generally, a 1% drop in weight can reduce blood pressure by 1-2 mm Hg.25
Cancer
Overweight and obesity are linked to an increased risk of various cancers, particularly hormone-dependent and gastrointestinal cancers.4 The mechanisms behind this increased risk are multifaceted. Firstly, excess fat tissue causes chronic inflammation, which can damage DNA and promote cancer growth. Obesity also leads to hormonal imbalances, like higher levels of insulin and oestrogen, which increase the risk of cancers such as breast and endometrial cancer.26 Fat tissue releases substances like leptin, which encourages cell growth and has lower levels of adiponectin, which fights inflammation.
Additionally, obesity increases oxidative stress and weakens the immune system, making it harder to fight cancer. 27 These factors contribute to a higher risk of 13 types of cancer, including those of the colon, breast (postmenopausal), and pancreas.
Osteoarthritis
The most significant impact of obesity on the musculoskeletal system is associated with osteoarthritis, a condition that causes joint pain, stiffness, and reduces your ability to move, significantly affecting quality of life.28
Degenerative diseases of the weight-bearing joints, such as the knee, are common complications of overweight and obesity. Mechanical damage to joints resulting from excess weight is generally thought to be the cause.28 Pain in the lower back is also more common in people living with obesity and may be one of the major contributors to obesity-related absenteeism from work.30
Asthma
Obesity is closely linked to an increased risk of asthma due to several interconnected mechanisms. Chronic low-grade inflammation caused by excess fat tissue leads to higher levels of substances that can worsen airway inflammation and sensitivity, which are key features of asthma.31
Additionally, the mechanical impact of excess weight, particularly around the abdomen, can reduce lung volumes and increase the work of breathing, worsening asthma symptoms. Hormonal imbalances, such as elevated leptin levels and reduced adiponectin levels, further contribute to airway inflammation. Metabolic disturbances common in obesity, including insulin resistance, also play a role in exacerbating asthma through increased oxidative stress and inflammation.
Can overweight people get pregnant?
Individuals with overweight can get pregnant, but there are important considerations to keep in mind. Obesity can affect fertility by causing hormonal imbalances, which may disrupt the menstrual cycle and ovulation. It can also increase the risk of complications during pregnancy and childbirth, such as gestational diabetes, preeclampsia, and the need for caesarean delivery.32
Moreover, excess body weight can impact the success rates of fertility treatments, such as in vitro fertilization (IVF). The WHO highlights that maintaining a healthy weight through balanced nutrition and physical activity is crucial for improving reproductive health and outcomes.33
How can obesity be prevented?
Obesity and related NCDs can be prevented and managed through individual and societal measures.34 For individuals, adopting healthy habits throughout life is crucial. This includes appropriate weight management during pregnancy, exclusive breastfeeding for the first six months, and continued breastfeeding up to 24 months or longer. Additionally, encouraging children to develop healthy eating habits, staying physically active, reducing screen time and other sedentary behaviours, and maintaining good sleep hygiene is important regardless of their current weight. Making healthier lifestyle choices, such as following a balanced diet, staying physically active, ensuring adequate sleep, and avoiding tobacco and excessive alcohol, is essential. Reducing the intake of total fats and sugars while increasing the consumption of fruits, vegetables, legumes, whole grains, and nuts supports overall health and well-being.
Health practitioners play a key role in obesity prevention by assessing the weight and height of patients, providing counselling on healthy diets and lifestyles, and offering integrated obesity prevention and management services.35 This includes advice on diet, physical activity, and medical or surgical measures when necessary. Monitoring other NCD risk factors, such as blood glucose, lipids, and blood pressure, and assessing the presence of comorbidities and disabilities, including mental health disorders, is also important.
Addressing obesity requires a multisectoral approach involving food manufacturing, marketing, and pricing. Policies and actions should focus on creating healthy food environments, making nutritious options more available, accessible, and desirable. Health sector responses should be designed to identify risks, prevent, treat, and manage obesity, integrating these efforts into broader NCD strategies and strengthening health systems through a primary healthcare approach.
The food industry, policy makers and other food system stakeholders can significantly contribute to promoting healthy diets by reducing the fat, sugar, and salt content of processed foods, ensuring that healthy and nutritious choices are available and affordable for all consumers, restricting the marketing of unhealthy foods, especially to children and teenagers, and supporting regular physical activity in the workplace.

Fig. 2 – Tips to prevent overweight and obesity throughout the life course.
Summary
Obesity is characterized by excessive fat accumulation, posing significant health risks. These risks are linked to genetics, dietary habits, and sedentary lifestyles. Addressing these factors through balanced diets, physical activity, and societal interventions is important to mitigate its health and economic burdens. Importantly, no single intervention can halt the rise of the growing obesity epidemic.
The article was developed in collaboration with the BETTER4U project. This project has received funding from the European Union’s Horizon Europe research and innovation programme under grant agreement No 101080117.
Visit www.better4u.eu for more info.


References
- Busetto, L., Dicker, D., Frühbeck, G., et al. (2024). A new framework for the diagnosis, staging and management of obesity in adults. *Nature Medicine*.
- 2. World Health Organization. (n.d.). Obesity. https://www.who.int/health-topics/obesity#tab=tab_1
- Rosen H. (2014). Is Obesity A Disease or A Behavior Abnormality? Did the AMA Get It Right?. Missouri medicine, 111(2), 104–108.
- World Health Organization. (2022). European regional obesity report 2022. https://iris.who.int/bitstream/handle/10665/353747/9789289057738-eng.pdf?sequence=1
- Rosen, H. (2014). Is obesity a disease or a behavior abnormality? Did the AMA get it right?. Missouri medicine, 111(2), 104.
- World Health Organization. (2022). European regional obesity report 2022. https://iris.who.int/bitstream/handle/10665/353747/9789289057738-eng.pdf?sequence=1
- Rosen, H. (2014). Is obesity a disease or a behavior abnormality? Did the AMA get it right?. Missouri medicine, 111(2), 104
- European Association for the Study of Obesity. (n.d.). 12 causes of obesity. https://easo.org/12-causes-of-obesity/
- Moschonis, G., & Trakman, G. L. (2023). Overweight and Obesity: The Interplay of Eating Habits and Physical Activity. Nutrients, 15(13), 2896. https://doi.org/10.3390/nu15132896
- https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017 Jun;6(2):187-194. doi: 10.1007/s13679-017-0262-y. PMID: 28455679; PMCID: PMC5497590.
- Mahmoud, R., Kimonis, V., & Butler, M. G. (2022). Genetics of Obesity in Humans: A Clinical Review. International journal of molecular sciences, 23(19), 11005. https://doi.org/10.3390/ijms231911005
- Obesity Medicine Association. (n.d.). Obesity and genetics. https://obesitymedicine.org/blog/obesity-and-genetics/
- Faith, M. S., & Kral, T. V. E. (2006). Social environmental and genetic influences on obesity and obesity-promoting behaviors: Fostering research integration. In L. M. Hernandez & D. G. Blazer (Eds.), Genes, behavior, and the social environment: Moving
- Kobylińska M, Antosik K, Decyk A, Kurowska K. Malnutrition in Obesity: Is It Possible? Obes Facts. 2022;15(1):19-25. doi: 10.1159/000519503. Epub 2021 Nov 8. PMID: 34749356; PMCID: PMC8820192.
- Herbst, K. L. (2019, December 14). Subcutaneous adipose tissue diseases: Dercum disease, lipedema, familial multiple lipomatosis, and Madelung disease. In K. R. Feingold, B. Anawalt, M. R. Blackman, et al. (Eds.), Endotext [Internet]. MDText.com, Inc.
- Caleyachetty R, Barber TM, Mohammed NI, Cappuccio FP, Hardy R, Mathur R, Banerjee A, Gill P. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2021 Jul;9(7)
- Obesity Action Coalition. (n.d.). Obesity and type 2 diabetes. https://www.obesityaction.org/resources/obesity-and-type-2-diabetes/
- Wondmkun Y. T. (2020). Obesity, Insulin Resistance, and Type 2 Diabetes: Associations and Therapeutic Implications. Diabetes, metabolic syndrome and obesity : targets and therapy, 13, 3611–3616. https://doi.org/10.2147/DMSO.S275898
- Obradovic M, Sudar-Milovanovic E, Soskic S, Essack M, Arya S, Stewart AJ, Gojobori T, Isenovic ER. Leptin and Obesity: Role and Clinical Implication. Front Endocrinol (Lausanne). 2021 May 18;12:585887. doi: 10.3389/fendo.2021.585887. PMID: 34084149; PM
- Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes. 2012 Apr;19(2):81-7. doi: 10.1097/MED.0b013e3283514e13. PMID: 22327367; PMCID: PMC4038351.
- Dludla PV, Mabhida SE, Ziqubu K, Nkambule BB, Mazibuko-Mbeje SE, Hanser S, Basson AK, Pheiffer C, Kengne AP. Pancreatic β-cell dysfunction in type 2 diabetes: Implications of inflammation and oxidative stress. World J Diabetes. 2023 Mar 15;14(3):130-14
- Cercato, C., & Fonseca, F. A. (2019). Cardiovascular risk and obesity. Diabetology & Metabolic Syndrome, 11, 74. https://doi.org/10.1186/s13098-019-0468-0
- Manrique-Acevedo, C., Chinnakotla, B., Padilla, J., Martinez-Lemus, L. A., & Gozal, D. (2020). Obesity and cardiovascular disease in women. International Journal of Obesity, 44(6), 1210-1226. https://doi.org/10.1038/s41366-020-0548-0
- Das, P., & Ingole, N. (2023). Lipoproteins and their effects on the cardiovascular system. Cureus, 15(11), e48865. https://doi.org/10.7759/cureus.48865
- Mills, K. T., Stefanescu, A., & He, J. (2020). The global epidemiology of hypertension. Nature reviews. Nephrology, 16(4), 223–237. https://doi.org/10.1038/s41581-019-0244-2
- Shantha, G. P. S., Kumar, A. A., Kahan, S., Cheah, S. Y., & Cheskin, L. J. (2013). Intentional weight loss and dose reductions of antihypertensive medications: a retrospective cohort study. Cardiorenal medicine, 3(1), 17–25. https://doi.org/10.1159/000
- Zhong, W., Wang, X., Wang, Y., Sun, G., Zhang, J., & Li, Z. (2023). Obesity and endocrine-related cancer: The important role of IGF-1. Frontiers in endocrinology, 14, 1093257. https://doi.org/10.3389/fendo.2023.1093257
- Jovanović, M., Kovačević, S., Brkljačić, J., & Djordjevic, A. (2023). Oxidative Stress Linking Obesity and Cancer: Is Obesity a 'Radical Trigger' to Cancer?. International journal of molecular sciences, 24(9), 8452. https://doi.org/10.3390/ijms24098452
- King, L. K., March, L., & Anandacoomarasamy, A. (2013). Obesity & osteoarthritis. The Indian journal of medical research, 138(2), 185–193.
- National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Health risks of overweight & obesity. https://www.niddk.nih.gov/health-information/weight-management/adult-overweight-obesity/health-risks?dkrd=/health-information/weight-managem
- Peters, U., Dixon, A. E., & Forno, E. (2018). Obesity and asthma. The Journal of allergy and clinical immunology, 141(4), 1169–1179. https://doi.org/10.1016/j.jaci.2018.02.004
- Catalano, P. M., & Shankar, K. (2017). Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ (Clinical research ed.), 356, j1. https://doi.org/10.1136/bmj.j1
- Hamad, F. T., & Chaalala, C. (2022). Effect of obesity on male fertility and its management. Middle East Fertility Society Journal, 27(1), Article 39. https://doi.org/10.1186/s43043-022-00126-2
- Budreviciute, A., Damiati, S., Sabir, D. K., Onder, K., Schuller-Goetzburg, P., Plakys, G., Katileviciute, A., Khoja, S., & Kodzius, R. (2020). Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Frontiers
- Fruh, S., Williams, S., Hayes, K., Hauff, C., Hudson, G. M., Sittig, S., Graves, R. J., Hall, H., & Barinas, J. (2021). A practical approach to obesity prevention: Healthy home habits. Journal of the American Association of Nurse Practitioners, 33(11),



