Europe’s obesity statistics: figures, trends & rates by country
Last Updated : 17 October 2024Key takeaways:
- Over 1 billion people worldwide live with obesity, including ~880 million adults and ~159 million children.
- In the EU, 53% of adults are overweight, with rates higher among men and older age groups. A higher educational level is also linked to a lower obesity risk among women.
- Overweight and obesity rates vary greatly across countries, with Romania, Poland, Croatia, and Slovakia having the highest prevalence among men, while Ireland, Romania, and Croatia have the highest prevalence among women. France has the lowest prevalence for both.
- Obesity is rising in adults and children due to obesogenic environments related to limited access to affordable healthy foods, fewer opportunities for daily physical activity, and insufficient supportive policies and regulations.
- Overweight and obesity contribute to premature death and disability, being responsible for ~13% of early deaths in Europe. If we added up all the years Europeans lived with obesity-related health problems in 2019, it would total nearly 8.7 million years.
- The economic burden of overweight and obesity is high, costing Europe ~€464 billion in 2019, with costs expected to more than double by 2060.
Obesity is a complex, multifactorial disease, defined as abnormal or excessive accumulation of fat that poses a health risk.1It has been recognised as a major public health concern and a significant contributor to death and disability. Obesity is a key risk factor in the development of many non-communicable diseases such as cardiovascular diseases, type 2 diabetes, hypertension, coronary heart diseases, and certain cancers. The Body Mass Index (BMI) scale is used to screen for obesity and used together with other factors to diagnose obesity.
This article presents data on overweight and obesity – its prevalence, trends over time, drivers, health consequences, and associated healthcare costs.
Obesity rates by country
Overweight and obesity rates vary significantly from country to country, between different population groups, across different age groups and sex, and also according to socioeconomic factors such as income, education, employment status, and place of residence.1
Estimates from 2022 come from the NCD Risk Factor Collaboration, a network of health scientists around the world that provide data on risk factors for non-communicable diseases (NCDs). According to their estimates, worldwide, more than one billion people are living with obesity. This includes about 880 million adults and 159 million children.2 Nearly 53% of the adult (aged 18 and over) EU's population were classified as overweight in 2019. The proportion of overweight men was consistently higher than the one for women.3
When analysing the share of the population by age groups, we see an increase in the proportion of population that was overweight with increasing age. Ages 18-24 had the lowest shares of overweight (25.0%), while ages 65-74 had the highest shares of overweight (65.7%) (with the exception of a few countries).3
A trend was also noticed by educational level: as the education level of women rose, the proportion considered as being overweight fell. This was the case in all EU Member States. This clear pattern linking educational attainment levels and being overweight was not observed among males.3
When further examining the overweight and obesity prevalence in the EU, the data reveals large differences between countries, both for men and women. However, it is important to note that countries often use a different methodology, therefore comparing studies on the prevalence of overweight and obesity remains difficult.
For men, Romania and Poland lead with a 76% prevalence rate (of which 38% and 32% were living with obesity, respectively), closely followed by Croatia and Slovakia, each reporting a 74% prevalence (of which 35% and 31% were living with obesity, respectively). France has the lowest overweight and obesity prevalence among men at 41% (of which 10% were living with obesity), followed by the Netherlands at 54% (of which 15% were living with obesity) and Denmark at 56% (of which 16% were living with obesity).2
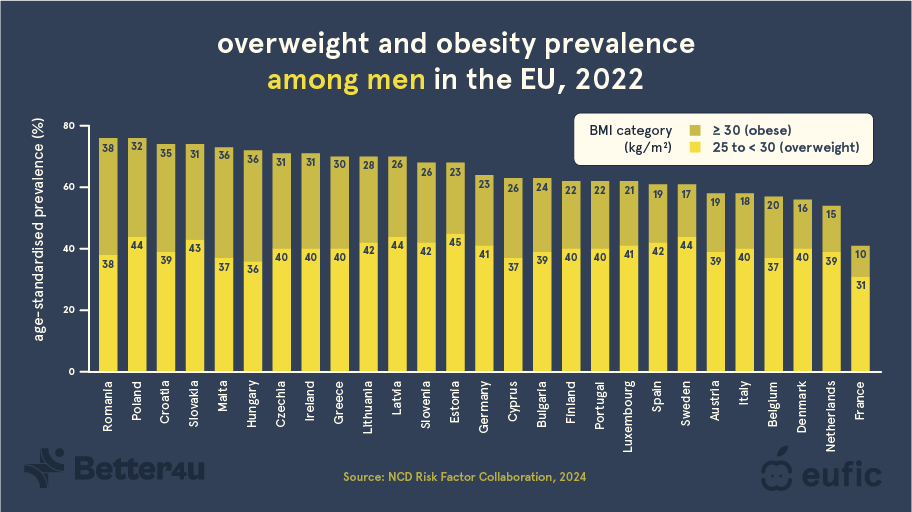
Fig. 1 – Overweight and obesity by country rates among men in the EU, 2022.2
For women, Ireland has the highest prevalence of overweight and obesity (62%, of which 28% were living with obesity) followed by Romania (58%, of which 32% were living with obesity), and Croatia (58%, of which 28% were living with obesity). Similarly, France has the lowest overweight and obesity prevalence among women at 30% (of which 10% were living with obesity), followed by Austria at 34% (of which 13% were living with obesity) and Denmark at 36% (of which 11% were living with obesity).2
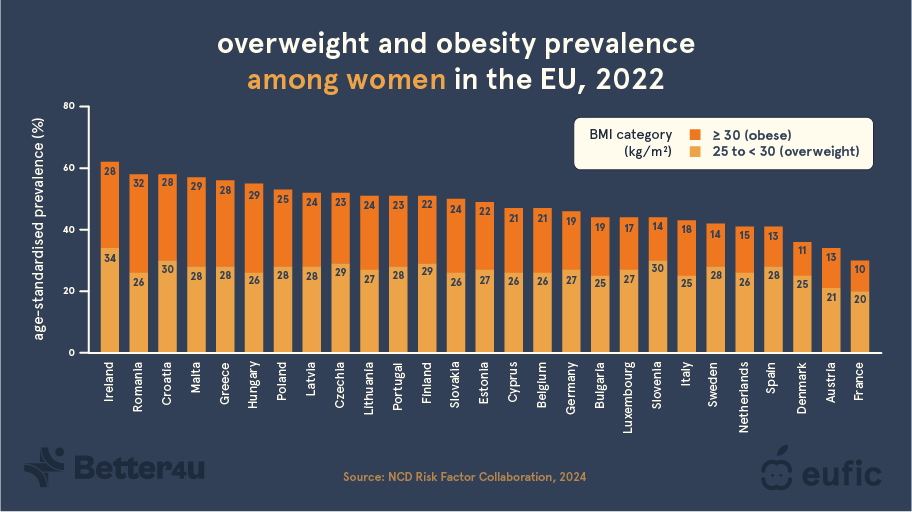
Fig. 2 – Overweight and obesity rates by country among women in the EU, 2022.2
There is no simple answer to explain why the overweight and obesity rates significantly vary between countries. A possible explanation could be due to differences in socioeconomic characteristics and the way these characteristics are measured. It has been found that people with a low socioeconomic status are more likely to be living with obesity. The socioeconomic status may indirectly influence weight status through dietary habits, good access to exercise facilities, health literacy, and levels of physical activity.4 Other possible explanations could include differences in dietary habits, urbanisation, cultural norms and perceptions, government policies and public health initiatives, and genetics and nutrigenetic interactions (i.e., how a person’s genes can affect the way their body responds to different foods, influencing their risk for health problems like overweight and obesity). For example, urban areas are often less activity-promoting and provide more access to unhealthy foods, promoting the development of overweight and obesity.1
You can learn more about the causes of obesity in this article.
Why is obesity increasing?
The prevalence of overweight and obesity is rising dramatically in children as well as in adults. Between 1975 and 2016, the prevalence of obesity in Europe rose 138%, with a 21% rise between 2006 and 2016.1 The prevalence of overweight rose by 51% between 1975 and 2016, and by 8% between 2006 and 2016. It is expected that by 2030, over half of Europe will live with obesity – up to 89% in some countries. No Member State is on track to reach the target of halting the rise in obesity by 2025.1,5
Obesity is a complex disease with many causes. Obesity and overweight result from an imbalance of energy intake (diet) and energy expenditure (physical activity), with extra calories being stored in the body as fat. However, the causes of obesity are much more complex than just the combination of an unhealthy diet and physical inactivity.1 It is caused by the interaction between biological, genetic, social, psychological, and environmental factors.6
The rise in overweight and obesity is largely due to changing environments to so-called obesogenic environments.1 Obesogenic environments promote overweight and obesity by limiting the availability of healthy, sustainable food at locally affordable prices, a lack of opportunities for people to engage in physical activity in daily life, and a lack of adequate legal and regulatory environments. Since the COVID-19 pandemic and the war in Ukraine, there has been a rise in both poverty and food prices, particularly for nutrient-rich foods.2 Along with the negative effects of climate change on food production and supply, these factors increase the prevalence of obesity by driving consumers to switch to less healthy foods. At the same time, we are moving less and less – possibly because of changes in work and transportation – which may have contributed to the rise in obesity. Marketing of unhealthy foods and beverages, especially targeting vulnerable populations like children, and the rise of sedentary online gaming also contribute to rising obesity rates.1 This is especially concerning since research suggests that children with obesity have a higher chance of becoming adults with obesity and are more likely to develop non-communicable diseases in later life.1
Why is obesity a problem?
What are the health consequences of overweight and obesity?
Overweight and obesity are among the leading risk factors in the development of many non-communicable diseases (NCDs) and are also associated with early death.1 People living with obesity also face weight bias, stigma, discrimination, and challenges accessing empathetic, evidence-based healthcare.
Some medical conditions associated with obesity include:1
- Cardiovascular diseases, including stroke, ischemic heart disease, heart failure, hypertensive heart disease, dyslipidaemia (abnormal high levels of lipids (fats) in the blood), and hypertension.
- Chronic respiratory diseases, including chronic obstructive pulmonary disease, obstructive sleep apnoea, and asthma.
- Cancer, including those of the breast, colorectum, gallbladder, stomach, kidney, liver, pancreas, uterus, ovary, oesophagus and thyroid, and multiple myeloma and meningioma.
- Chronic kidney disease.
- Mental health problems, such as depression.
- Musculoskeletal complications, including low back pain and osteoarthritis.
- Non-alcoholic fatty liver disease.
- Type 2 diabetes.
Around 1.24 million people (or 13%) in Europe in 2019 had a premature death as a result of overweight and obesity. This marks overweight and obesity as the fourth leading cause of death, after having high blood pressure, dietary risks (e.g., diets low in whole grains, legumes, and fruit and high in sodium, processed meat, and red meat), and smoking.7 On average, overweight and obesity reduce life expectancy by nearly three years.8 A high BMI is also the leading risk factor for years lived with disability, being responsible for 7% (or nearly 8.7 million) of total years lived with disability.7 In other words, almost 8.7 million years of healthy life were lost due to ill-health related to having a high BMI.
It is estimated that 80% of cases of type 2 diabetes, 35% of ischaemic heart disease, and 55% of high blood pressure cases among adults in Europe are attributable to overweight and obesity.9 Furthermore, across Europe, obesity is likely to be directly responsible for at least 200.000 new cancer cases annually and this figure is expected to rise further in the coming decades.1 Obesity may even surpass smoking as the leading risk factor for cancer in some countries in the future.10 Overweight and obesity also increase the risk of intensive care admissions and death from COVID-19.11 In fact, obesity is linked with more than 200 comorbidities.12
What is the economic cost of overweight and obesity?
Obesity and overweight also pose a huge and growing financial burden on national resources and healthcare systems. Overweight and obesity both have direct costs, including direct medical costs (e.g., costs of personal health care, hospital care, physician services and drugs for diseases with a well-established relationship with obesity) and direct non-medical costs (e.g., travel costs and informal caregiver travel costs), and indirect non-medical costs, including the costs of premature mortality and productivity losses.13
In 2019, it was estimated that overweight and obesity cost Europe an amount approximately equal to €464 billion euros, of which approximately €141 billion euros were through direct costs and approximately €323 billion euros through indirect costs (calculated from US dollars to euros). Total costs per capita were equal to approximately €499 euros and total costs as a percentage of GDP were equal to 2.16%. Predictions indicate that the associated costs of overweight and obesity will more than double between 2020 and 2060.13
The European Association for the Study of Obesity (EASO) found direct obesity-related costs ranging from 1.5 to 4.6% of health expenditure in France to around 7% in Spain.14 However, predictions indicate that if European governments focused all of their current and future weight management funding on the most cost-effective strategies, governments could save as much as 60% in some countries.15
You can learn more about how obesity can be prevented here.
Summary
Overweight and obesity are a significant public health problem. Recent estimates indicate that now over a billion people are living with obesity, including 880 million adults and 159 children, and is still on the rise. In Europe, the prevalence of overweight and obesity differs by country, with Romania, Poland, Croatia, and Slovakia having the highest prevalence among men, while Ireland, Romania, and Croatia have the highest prevalence among women. For society as a whole, this is associated with both direct and indirect costs and puts a strain on healthcare and social resources. These figures underscore the urgency for collective action and tailored interventions to reverse this trend.
The article was developed in collaboration with the BETTER4U project. This project has received funding from the European Union’s Horizon Europe research and innovation programme under grant agreement No 101080117.
Visit www.better4u.eu for more info.


References
- World Health Organization. (2022). WHO European regional obesity report 2022. World Health Organization. Regional Office for Europe.
- Phelps, N. H., Singleton, R. K., Zhou, B., Heap, R. A., Mishra, A., Bennett, J. E., ... & Barbagallo, C. M. (2024). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 milli
- Eurostat. (2024). Overweight and obesity – BMI statistics. Accessed 23 September 2024.
- Marques, A., Peralta, M., Naia, A., Loureiro, N., & de Matos, M. G. (2018). Prevalence of adult overweight and obesity in 20 European countries, 2014. The European Journal of Public Health, 28(2), 295-300.
- World Health Organization. (2021). Monitoring noncommunicable disease commitments in Europe 2021: are we on track to reach targets 10 years after the Moscow Declaration and First United Nations High-Level Meeting?. In Monitoring noncommunicable disease
- EASO. (2019). 12 causes of obesity. Accessed 14 May 2024
- IHME. (2019). Global Burden of Disease. Accessed 8 May 2024.
- OECD/European Union (2020), Health at a Glance: Europe 2020: State of Health in the EU Cycle, OECD Publishing, Paris.
- World Health Organization. (2007). The challenge of obesity in the WHO European Region and the strategies for response. World Health Organization. Regional Office for Europe.
- Cancer Intelligence Team. (2018). When could overweight and obesity overtake smoking as the biggest cause of cancer in the UK? Oxford: Cancer Research UK.
- Popkin, B. M., Du, S., Green, W. D., Beck, M. A., Algaith, T., Herbst, C. H., ... & Shekar, M. (2020). Individuals with obesity and COVID‐19: a global perspective on the epidemiology and biological relationships. Obesity reviews, 21(11), e13128.
- Yuen, M. M. (2023). Health complications of obesity: 224 obesity-associated comorbidities from a mechanistic perspective. Gastroenterology Clinics, 52(2), 363-380.
- Okunogbe A, et al. (2022). Economic impacts of overweight and obesity: current and future estimates for 161 countries. BMJ global health, 7(9), e009773.
- EASO. (2023). World Obesity Day Key Messages. Accessed 16 May 2024.
- Erixon F, Brandt L, & Krol M. (2014). Investing in obesity treatment to deliver significant healthcare savings: estimating the healthcare costs of obesity and the benefits of treatment. European Centre for International Political Economy.



